Patient burden and epidemiology
Heart failure (HF) with LVEF >40% has a substantial impact on patients' quality of life:1,2
High symptom burden3
Reduced daily functioning1,2
Physical impairment1,3
Poor mental health1
People with HF often require family/caregiver support. Caregivers of people with HF report experiencing physical, psychological, social, professional and economic challenges.5,6
7
Risk factors and pathophysiology
HFrEF, HFmrEF, and HFpEF share several risk factors
and common comorbidities.14
↑ and ↓ denote higher or more common and lower or less common, respectively, than in an age-matched control population, with the exception of age, in which ↑ denotes higher than average among adults.
Phenotype
Age
Women
Ischemic heart disease
Atrial fibrillation
Hypertension
Chronic kidney disease
Natriuretic peptide levels
HFrEF - LVEF ≤40%
HFmrEF - LVEF 41–49%
HFpEF - LVEF ≥50%
HFpEF is particularly associated with increasing age, atrial fibrillation, hypertension and chronic kidney disease15
↑ and ↓ denote higher or more common and lower or less common, respectively, than in an age-matched control population, with the exception of age, in which ↑ denotes higher than average among adults.
HFrEF - LVEF ≤40%
Phenotype
Age
Women
Ischemic heart disease
Atrial fibrillation
Hypertension
Chronic kidney disease
Natriuretic peptide levels
HFmrEF - LVEF 41–49%
Phenotype
Age
Women
Ischemic heart disease
Atrial fibrillation
Hypertension
Chronic kidney disease
Natriuretic peptide levels
HFpEF - LVEF ≥50%
Phenotype
Age
Women
Ischemic heart disease
Atrial fibrillation
Hypertension
Chronic kidney disease
Natriuretic peptide levels
Adapted from Savarese et al, Heart failure with mid-range or mildly reduced ejection fraction, Nature Reviews, Cardiology, Vol 19, page 102, 2022 Springer Nature.

Diagnosis
Definition of heart failure18
Heart failure is a clinical syndrome with current or prior symptoms and/or signs caused by a structural and/or functional cardiac abnormality and is supported by at least one of the following:
- Elevated natriuretic peptide levels
- Objective evidence of cardiogenic pulmonary or systemic congestion
During initial assessment of patients with suspected HF:9
- Clinical history should be assessed.
- Physical examination helps to identify factors that might accelerate the development or progression of heart failure (e.g. lifestyle or behavioral factors).
- Electrocardiogram (ECG) and laboratory evaluation should be performed.
- Measurement of biomarkers (e.g. B-type natriuretic peptide (BNP), N-terminal prohormone of B-type natriuretic peptide (NT-proBNP), cardiac troponin) are useful to support diagnosis.
Laboratory evaluation9
- Complete blood count
- Urinalysis
- Serum electrolytes
- Blood urea nitrogen
- Serum creatinine
- Glucose
- Fasting lipid profile
- Liver function tests
- Iron studies
- Thyroid-stimulating hormone level
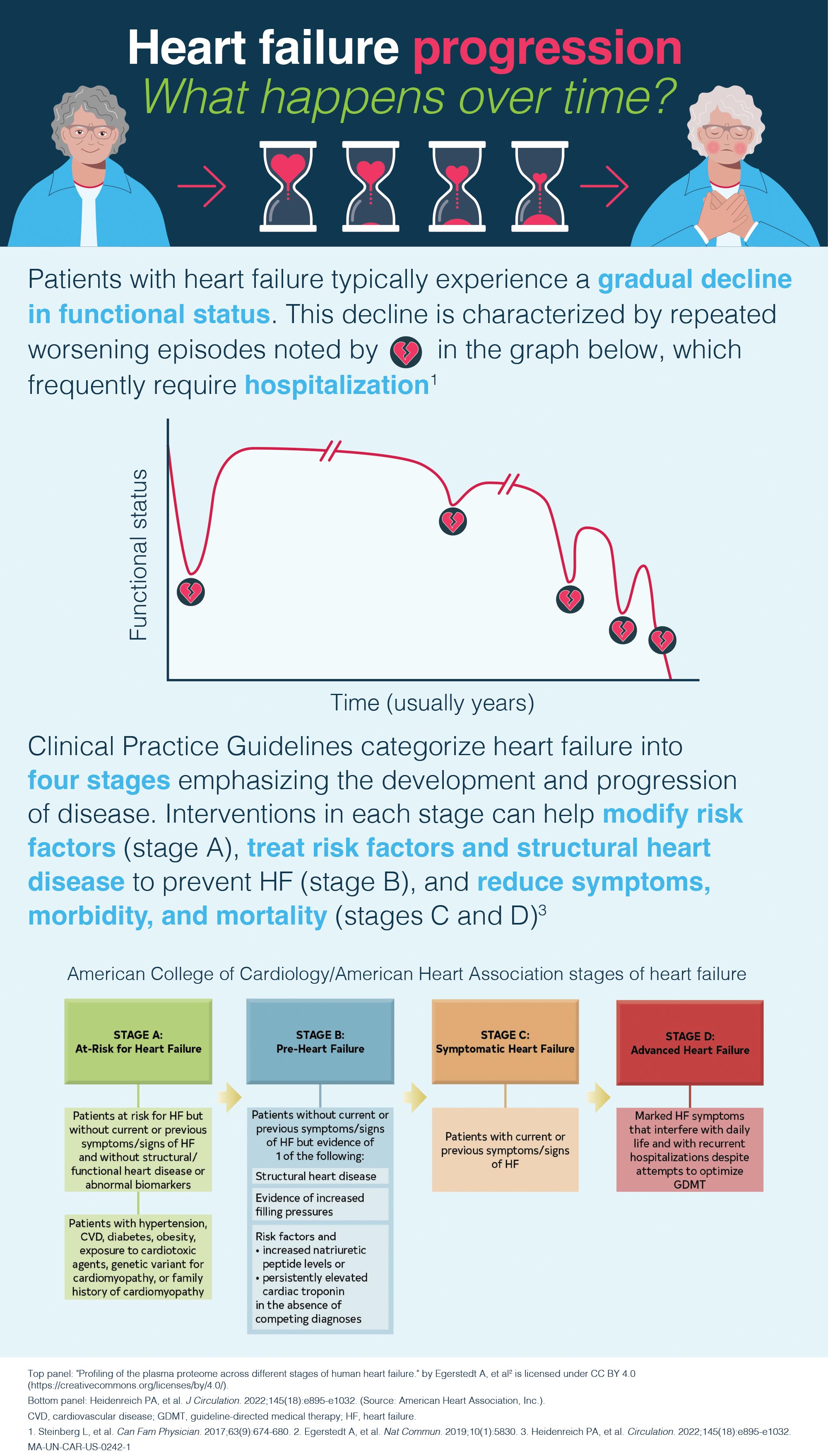
Disease management
Current guideline-directed medical therapy (GDMT) for HF with LVEF >40% involves lifestyle modifications and pharmacologic therapy to reduce congestion (diuretics) and treat underlying conditions.9
Early diagnosis and treatment of HF with LVEF >40% may delay disease progression and improve patient outcomes.24,25

If you would like more information on Bayer's scientific and clinical advances, please
Contact us Visit our US Medical Affairs websiteThis platform offers information on earlier intervention to lower CV risk and improve outcomes in your patients with chronic kidney disease (CKD) associated with type 2 diabetes (T2D).
Explore a variety of educational resources to...
Hear expert clinical perspectives on topics including CV risk in CKD/T2D
Learn about the CV and renal risks linked to albuminuria
Recognize the impact and burden of CKD/T2D
Discover the benefits of albuminuria reduction on patient outcomes
1. Warraich HJ, Kitzman DW, Whellan DJ, Duncan PW, Mentz RJ, Pastva AM, et al. Physical Function, Frailty, Cognition, Depression, and Quality of Life in Hospitalized Adults >/=60 Years With Acute Decompensated Heart Failure With Preserved Versus Reduced Ejection Fraction. Circ Heart Fail. 2018;11(11):e005254. 2. Chandra A, Vaduganathan M, Lewis EF, Claggett BL, Rizkala AR, Wang W, et al. Health-Related Quality of Life in Heart Failure With Preserved Ejection Fraction: The PARAGON-HF Trial. JACC Heart Fail. 2019;7(10):862-74. 3. Nguyen C, Bamber L, Willey VJ, Evers T, Power TP, Stephenson JJ. Patient Perspectives on the Burden of Heart Failure with Preserved Ejection Fraction in a US Commercially Insured and Medicare Advantage Population: A Survey Study. Patient Prefer Adherence. 2023;17:1181-96. 4. McHorney CA, Mansukhani SG, Anatchkova M, Taylor N, Wirtz HS, Abbasi S, et al. The impact of heart failure on patients and caregivers: A qualitative study. PLoS ONE. 2021; 16(3): e0248240. 5. Pressler SJ, Gradus-Pizlo I, Chubinski SD, Smith G, Wheeler S, Wu J, et al. Family caregiver outcomes in heart failure. Am J Crit Care. 2009;18(2):149-59. 6. Suksatan W, Tankumpuan T, Davidson PM. Heart Failure Caregiver Burden and Outcomes: A Systematic Review. J Prim Care Community Health. 2022;13:21501319221112584. 7. McHorney CA, Mansukhani SG, Anatchkova M, Taylor N, Wirtz HS, Abbasi S, et al. The impact of heart failure on patients and caregivers: A qualitative study. PLoS One. 2021;16(3):e0248240. 8. Bozkurt B, Ahmad T, Alexander K, Baker WL, Bosak K, Breathett K, et al. HF STATS 2024: Heart Failure Epidemiology and Outcomes Statistics An Updated 2024 Report from the Heart Failure Society of America. J Card Fail. 2025;31(1):66-116. 9. Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145(18):e895-e1032. 10. Vasan RS, Xanthakis V, Lyass A, Andersson C, Tsao C, Cheng S, et al. Epidemiology of Left Ventricular Systolic Dysfunction and Heart Failure in the Framingham Study: An Echocardiographic Study Over 3 Decades. JACC Cardiovasc Imaging. 2018;11(1):1-11. 11. Tsao CW, Lyass A, Enserro D, Larson MG, Ho JE, Kizer JR, et al. Temporal Trends in the Incidence of and Mortality Associated With Heart Failure With Preserved and Reduced Ejection Fraction. JACC Heart Fail. 2018;6(8):678-85. 12. Shah KS, Xu H, Matsouaka RA, Bhatt DL, Heidenreich PA, Hernandez AF, et al. Heart failure with preserved, borderline, and reduced ejection fraction: 5-year outcomes. JACC. 2017; 70(20):2476-2486. 13. Nichols GA, Qiao Q, Linden S, Kraus BJ. Medical Costs of Chronic Kidney Disease and Type 2 Diabetes Among Newly Diagnosed Heart Failure Patients With Reduced, Mildly Reduced, and Preserved Ejection Fraction. Am J Cardiol. 2023;198:72-8. 14. Simmonds SJ, Cuijpers I, Heymans S, Jones EAV. Cellular and Molecular Differences between HFpEF and HFrEF: A Step Ahead in an Improved Pathological Understanding. Cells. 2020;9(1). 15. Savarese G, Stolfo D, Sinagra G, Lund LH. Heart failure with mid-range or mildly reduced ejection fraction. Nat Rev Cardiol. 2022;19(2):100-116. 16. Upadhya B, Kitzman DW. Heart failure with preserved ejection fraction: New approaches to diagnosis and management. Clin Cardiol. 2020;43(2):145-55. 17. O'Gallagher K, Shah AM. Modelling the complexity of heart failure with preserved ejection fraction. Cardiovasc Res. 2018;114(7):919-21. 18. Bozkurt B, Coats AJS, Tsutsui H, Abdelhamid M, Adamopoulos S, Albert N, et al. Universal definition and classification of heart failure. A report of the heart failure society of America, heart failure association of the European society of cardiology, Japanese heart failure society and writing committee of the universal definition of heart failure. J Card Fail. 2021;27(4):387-413. 19. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129-200. 20. Golla MSG, Shams P. Heart Failure With Preserved Ejection Fraction (HFpEF). StatsPearls[Internet]. Mar 2024. 21. Naing P, Forrester D, Kangaharan N, Muthumala A, Mon Myint S, Playford D. Heart failure with preserved ejection fraction: A growing global epidemic. Aust J Gen Pract. 2019;48(7):465-71. 22. Loke I, Antoniou S, Boramakot R, Walters D, Fuat A. Demystifying heart failure with a preserved ejection fraction: what you need to know. Br J Gen Pract. 2024;74(740):103-5. 23. American Heart Association (AHA). Ejection Fraction Heart Failure Measurement. 2025. [Available from: https://www.heart.org/en/health-topics/heart-failure/diagnosing-heart-failure/ejection-fraction-heart-failure-measurement]. 24. Jasinska-Piadlo A, Campbell P. Management of patients with heart failure and preserved ejection fraction. Heart. 2023;109(11):874-83. 25. Centers for Disease Control and Prevention. About Heart Failure 2024 [Available from: https://www.cdc.gov/heart-disease/about/heart-failure.html#cdc_disease_basics_treatment-treatment-and-recovery].